Engineers are essential to our health. From water purification and flood mitigation to surgical equipment and chemotherapy, they contribute across many specialties.
In countries around the world, severe resource limitations can get in the way of health and health care delivery—and the role engineers play can be even more crucial.
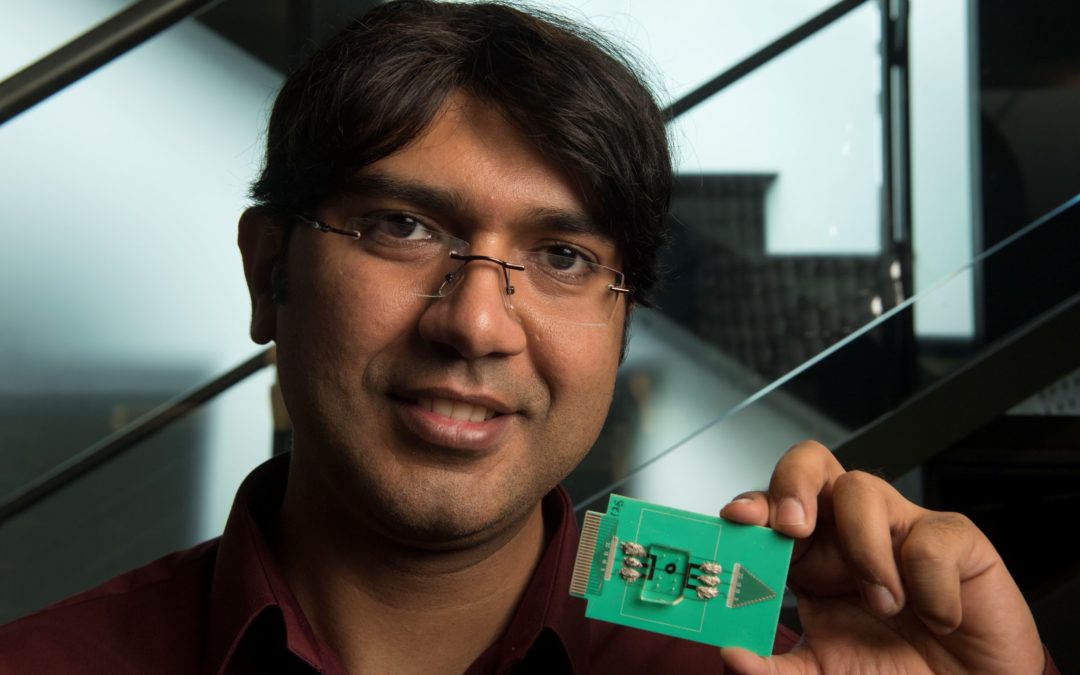
A pace-setter in this evolving field is Umer Hassan, a new faculty member in the School of Engineering with a joint appointment at Rutgers Global Health Institute. He is pursuing an interdisciplinary set of research initiatives at Rutgers that share a common goal: saving lives, particularly in vulnerable communities.
Engineering Meets Medicine Meets Global Health
Hassan, an assistant professor, is working with colleagues universitywide to apply his electrical and computer engineering expertise—which incorporates personalized medicine, predictive prognostic systems, and infectious disease—to solve pressing global health challenges.
One such challenge: sepsis, a life-threatening condition caused by the body’s response to infection.
Any kind of infection can potentially lead to sepsis—urinary tract infection, strep throat, influenza—and even routine surgeries create a risk. The human body’s complex response in sepsis can cause tissue damage, organ failure, and death. Sepsis survivors have described their pain as feeling like they were going to die.
In 2017, the World Health Organization identified as a global health priority the urgent need to improve the prevention, diagnosis, and management of sepsis. Hassan is designing a medical device that would bring to a patient’s bedside the capacity to diagnose sepsis—and do so quickly, accurately, inexpensively, and with minimal training required for health care providers.
Inexpensive Device Detects Sepsis Quickly and Accurately
WHO estimates that sepsis causes 6 million deaths worldwide every year, most of which are preventable. In lower- and middle-income countries, there may not even be a trained clinician available to draw a blood sample to test for sepsis, let alone a physician specialist capable of managing such a dynamic, life-threatening condition.
Intervention, by way of innovation, is desperately needed.
Hassan is actively engaged in the global effort to combat sepsis. “We are building an automated device that would cost less than $10 a test and is simple to operate. Many countries’ health systems cannot support large equipment and expensive technologies that require advanced training and knowledge to use,” he says.
Time and accurate diagnoses are critical factors in managing sepsis. Hassan is working across disciplines at Rutgers and with industry partners to identify new biomarkers and create machine-learning algorithms—essentially, artificial intelligence systems—that will “dramatically improve clinicians’ abilities to diagnose as well as predict sepsis,” he says. “Not only in resource-limited settings, but everywhere.”
Hassan’s findings were recently published in the journal Nature Communications, in a co-authored paper titled “A point-of-care microfluidic biochip for quantification of CD64 expression from whole blood for sepsis stratification.” This spring, he will teach an engineering course in which students will learn to develop applications for global health settings.
Photography by Nick Romanenko